Friday Report: Issue 53
By: John Roberts, Adele Groyer, Matt Fletcher and Nicola Oliver
COVID-19 Actuaries Response Group – Learn. Share. Educate. Influence.
 Covid-arg.com
Covid-arg.com
COVID-19 is still one of the hottest topics for scientific papers and articles. The COVID‑19 Actuaries Response Group provides a regular Friday update with a summary of key papers and articles.
Vaccines
Roll-out of Boosters
The roll-out of booster (and third primary) doses to those in Priority Groups 1 to 9 is now well under way. Currently the weekly rate in England is 1.2m doses, which might be regarded as disappointing in comparison with the 3m to 4m we saw during the earlier stages of the programme.
The latest figures show that in England we have given 3.1m a booster (including those for whom the 3rd dose is actually a completion of the primary course), with the Over 80 age group now up to 42% of those eligible. In parallel with the oldest age groups we are again focussing on health and care workers together with care home residents.
To put the 3.1m in context, there are currently 7.4m people who have passed the six month eligibility criteria to be boosted, and thus 4.3m are eligible, but yet to have, their 3rd dose.
In the latest UKHSA Vaccination Surveillance Report (link), data shows that over 1,400 in the 80+ age group who were fully vaccinated have died in the last four weeks. Later we’ll report on data that shows a potential ten-fold or more benefit from having the booster dose, so the importance of a faster roll-out is demonstrated by the deaths that can be saved in a relatively short period.
Progress in 12 to 15 Year Vaccination
Also in the Vaccination Surveillance Report, there’s an update on first vaccination of 12 to 15 year olds, where there’s slightly better progress than in prior weeks. However, the rate of climb of the graph is noticeably lower than that achieved in other age bands after they were opened up to general vaccination.
The pace of roll-out can be contrasted with that seen in Scotland, where 43% of 12 to 15 year olds have been vaccinated. North of the border a different model is being adopted in which children can be vaccinated at a drop-in centre, an option not available in England where schools are hosting vaccination by the local Schools Immunisation Services.

Israel Study on Booster Efficacy (link)
With Israel again at the forefront of global vaccination programmes, this time in respect of booster doses, it’s no surprise that it is first to start producing data on efficacy. A study of over 4m people between 30 July and 6 October concludes that the boosters reduce infection levels by a factor of 10, with an even greater reduction in serious illness and death.
As ever with this type of study, there is a risk of confounding factors distorting the result, in this case a possibility that those most risk averse are more likely to come forward for a booster.
The paper sets out how it has investigated this possibility with a secondary analysis, in which the experience of those boosted is studied, comparing the period immediately post vaccination (when there is assumed to be very little benefit from the booster), and after 12 days. This still shows a significant improvement in both infections and serious illness, albeit somewhat lower than the main investigation.
Pfizer efficacy over time and against variants
In this retrospective cohort study, funded by Pfizer, electronic health records of over 3.4m members of the health-care organisation Kaiser Permanente Southern California were used to assess BNT162b2 vaccine effectiveness against SARS-CoV-2 infections and COVID-19-related hospital admissions. The study period ran from 14 December 2020 to 8 August 2021.
Effectiveness against infections declined from 88% (95% CI 86–89) during the first month after full vaccination to 47% (43–51) after 5 months. Among sequenced infections, vaccine effectiveness against infections of the Delta variant was 93% (85–97) during the first month after full vaccination but declined to 53% (39–65) after 4 months. Effectiveness against other variants during the first month after full vaccination was also 97% (95–99), but waned to 67% (45–80) at 4–5 months.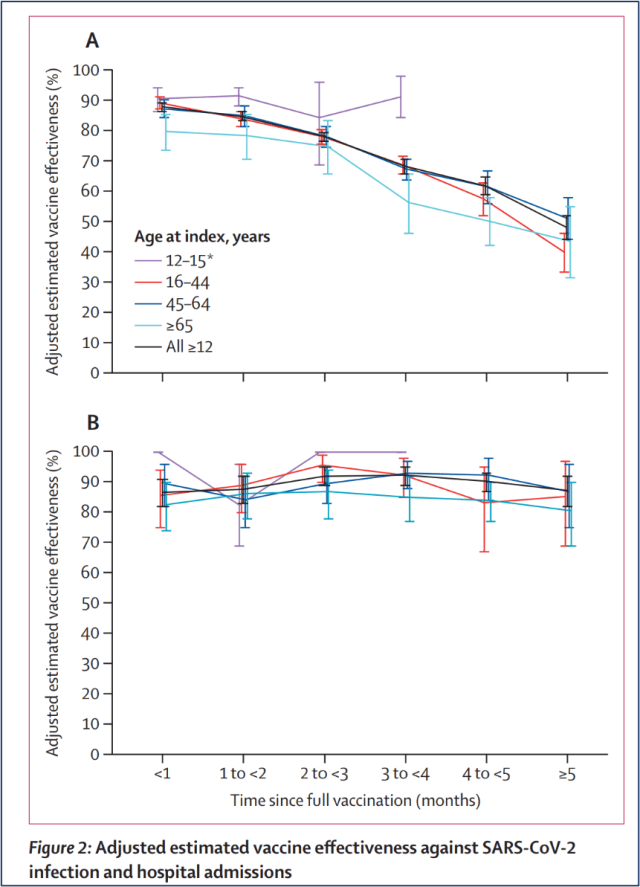
While it appears that the efficacy against Delta declined more rapidly, the difference in rate of decline in vaccine effectiveness between Delta and other variants was not statistically significant (p=0·30).
From this the authors proposed that reduction in vaccine effectiveness against SARS-CoV-2 infections is primarily due to waning immunity with time rather than the Delta variant specifically escaping vaccine protection.
Effectiveness against hospital admissions for infections with Delta was 93% (84–96) up to 6 months. Across all variants, there was little indication of waning of effectiveness against hospitalisation.
Variants
Diversity within the Delta variant
The UK Health Security Agency (UKHSA) monitors variants and their sublineages, and releases reports every two weeks. The latest report from 15 October (link) shows that the original B.1.617.2 Delta lineage was last dominant in late April. It was overtaken by AY.4 which remains dominant but there is evidence of competition from other lineages in recent weeks.
Additionally sublineage AY.4.2 which is a mutation of AY.4 has just been designated but is not yet shown in the Pangolin tool (link). UKHSA says that this sublineage, which includes spike mutations A222V and Y145H, is currently increasing in frequency. In the week beginning 27 September 2021, this sublineage accounted for approximately 6% of all sequences generated.
It is too soon to speculate whether this sublineage’s real-world impacts differ from those of other Delta lineages.

Clinical and medical news
Impact of circulating SARS-CoV-2 variants on mRNA vaccine-induced immunity
How does the SARS-CoV-2-specific adaptive immune response differ between that triggered by a vaccine and that triggered by infection in the face of emerging virus variants? Between November 2020 and January 2021, 40 healthcare workers were enrolled in a study which set out to do just that. Following receiving either the Moderna or the Pfizer COVID-19 vaccine, the group were stratified according to prior exposure to SARS-CoV-2 as either previously infected (recovered) or uninfected (naive). Blood samples were collected at baseline (prior to vaccination), 7- and 28- days post first vaccination dose, and 7-, 28- and 70-days post second vaccination dose.
The study authors report that despite faster and more prolific antibody responses to viral proteins in the recovered vs. the naïve group, vaccination led to overall similar levels of neutralizing antibodies after the second dose.
The study then examined the neutralization capacity of plasma samples from vaccinated individuals to 16 different locally circulating SARS-CoV-2 variants, including the variants of concern Alpha, Beta, Gamma, and Delta; former variants of interest, Epsilon B.1427 & B.1429, Eta, Iota, and Kappa; and lineages with key S gene mutations (B.1.517 with N501T, and B.1 and R.1 with E484K) using lineage A as a comparator. (The root of the pandemic lies within lineage A).
A range of responses was observed but, notably, previously infected individuals exhibited more significant neutralization activity against SARS-CoV-2 variants of concern than those without previous infection, even after both groups had received two vaccine doses. The authors suggest that future vaccine boosters (third dose) may help to overcome the reduction in neutralization capacity observed for those variants in which specific combinations of spike protein mutation in the receptor binding domain resulting in increased viral infectivity, virulence, and immune evasion potency.
Global prevalence and burden of depressive and anxiety disorders due to the pandemic
The Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) 2019 showed that the two most disabling mental disorders were depressive and anxiety disorders, both ranked among the top 25 causes of burden worldwide in 2019.
Given the potential impact of the pandemic on mental health, the COVID-19 Mental Disease Collaborators aimed to quantify the impact of the pandemic on the prevalence and burden of major depressive disorder and anxiety disorders globally in 2020. Using a systematic review of data, the team undertook meta-regression to estimate change in the prevalence of major depressive disorder and anxiety disorders between pre-pandemic and mid-pandemic.
Key findings include:
- Daily SARS-CoV-2 infection rates and reductions in human mobility were associated with increased prevalence of major depressive disorder and anxiety disorders;
- Females were affected more than males;
- Younger age groups were more affected than older age groups;
- The greatest increases in prevalence of major depressive disorder and anxiety were seen in geographical locations hit hardest by the pandemic.
In addition, the study calculated that an additional 53 million (CI 45 to 63m) cases of major depressive disorder globally (an increase of 28%) was due to the pandemic, as well as 76 million (CI 64 to 91m) cases of anxiety disorder (an increase of 26%).
Both major depressive disorder and anxiety disorders increase the risk of other diseases and suicide; the authors state that, ‘taking no action in the face of the estimated impact of the COVID-19 pandemic on the prevalence and burden of major depressive disorder and anxiety disorders should not be an option.’
Bamlanivimab plus Etesevimab in Mild or Moderate Covid-19
Bamlanivimab and Etesevimab are both neutralizing monoclonal antibodies which act through mimicking the immune system’s ability to fight off harmful pathogens, such as viruses like SARS-CoV‑2. These two compounds target the surface spike glycoprotein of SARS-CoV-2 that mediates viral entry into host cells.
Results from a phase 3 trial have recently been published in the NEJM. In the trial, high risk patients with mild or moderate COVID-19 were randomly assigned in a 1:1 ratio to receive a single intravenous infusion of either a neutralizing monoclonal-antibody combination agent (2,800 mg of bamlanivimab and 2,800 mg of etesevimab, administered together) or placebo within three days of a laboratory diagnosis of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection.
Early intervention with this drug combination resulted in a reduction in incidence of COVID-19–related hospitalization or death from any cause by day 29 compared with those who received placebo. It was also observed that the intervention accelerated a decline in the SARS-CoV-2 viral load.
Health and social well-being in the COVID-19 clinically vulnerable older population
Clinical vulnerability (‘CV’) is a term that is applied to those with specific health profiles and diseases (such as diabetes, lung and heart conditions). In those aged over 50 years who are CV, there is a concern that health and social well-being have been disproportionately affected. Using data from ELSA, this study examined these concerns through considering two main types of outcome during the pandemic: health, and social relationships and social engagement (‘social well-being’). All analyses controlled for a wide range of demographic and socioeconomic characteristics.
It was reported that:
- CV respondents who were shielding reported increased anxiety, depression, poor self-rated health and receipt of formal care as well as decreases in well-being and physical activity compared with those not CV and not shielding;
- Across different age groups, CV respondents were generally at greater risk of deterioration in health and social well-being compared with those in the same age group but without clinical vulnerabilities to COVID-19;
- Older people CV to COVID-19 were more likely to report worse health and social well-being outcomes during the pandemic compared with participants not CV, even taking into account pre-pandemic levels of health and social well-being.
Vaccinating against covid and flu at same time is safe
The “Combining Influenza and COVID-19 Vaccination” (ComFluCOV) study was designed to establish the safety of co-administering the most widely used COVID-19 and influenza vaccines in the UK and describe the expected side effects and immune responses to the vaccines when they are given together.
Results from this study have now been presented to the UK JCVI; it is reported that are no safety concerns combining the two vaccines, and that the immune response in both are preserved. The results are from a randomised trial in which 679 volunteers received their second dose of the COVID-19 vaccine and the flu vaccine at their first study visit then a saline injection (placebo) at their second visit; or received their second dose of the COVID-19 vaccine and a saline injection (placebo) at their first visit and then the flu vaccine at their second visit.
Note that the study did not exclude people who were pregnant, had severe uncontrolled medical problems, were immunocompromised, or aged 65 or over, so it was representative of the population who were most likely to receive both flu and covid vaccines.
Myocarditis Post Vaccination (link)
A study from Israel of over 2.5m people who had received at least one dose of the Pfizer vaccine has found that the overall rate of myocarditis within the first 42 days was 2.1 per 100,000. Notably, given the debate around vaccination of younger people, the risk was highest in the 16 to 29 year old male group, at 11 per 100,000.
Of the 54 cases, 51 of which were male, 76% were described as mild, and a further 22% as intermediate, leaving just 2% (1 case) which was associated with cardiogenic shock. One of the 54 patients died of an unknown cause following discharge; the study notes that they had pre-existing cardiac disease.

A second study, also from Israel (link), looked at the additional risk following the second dose. Whilst the overall results are slightly different, the same pattern of increased risk for younger adults, in particular males, was seen.

Effectiveness of Lateral Flow Tests (link)
The ability of lateral flow tests (LFTs) to pick up infected individuals has often been criticised as inadequate, when compared against the benchmark “gold standard” PCR tests, with a result as low as 40% in asymptomatic individuals mentioned. A new study looks at the test’s performance given the primary use of detecting infectious individuals in the community (eg school testing).
The study notes that PCR tests will record evidence of infection long after the individual has stopped shedding viral load (and is thus no longer infectious), and that this could amount to half of the cases where a positive result is obtained. Whilst these cases are important in terms of a clinical diagnosis, they are much less relevant in terms of public health measures, in particular in informing people that they must remove themselves from circulation to reduce spread.
Using the earlier 40% example (which related to mass testing in Liverpool, at the start of LFT use), the paper suggests that effectiveness “sensitivity” would have actually been over 80% when assessed against those who were infectious at the time of the test.
The paper notes other studies that are consistent with this conclusion, including CDC analysis which showed that LFT’s sensitivity rose from 41% (asymptomatic) and 80% (symptomatic) to 78% and 92% respectively when assessed against those with a positive viral culture.
Modelling
We first monitored actual hospitalisations in England against projections in Friday Report 48 (link). This updated our bulletin (link) summarising papers from London School of Hygiene and Tropical Medicine (LSHTM), Warwick University and Imperial College London which modelled the move to step 4.
The chart below shows an updated actual trajectory of hospitalisations in England against four of the projections produced by the groups:
- LSHTM central model (assuming waning immunity of 15% over the next 12 months)
- Warwick “green” and “pink” models which represent the two extremes of their assumptions on precautionary behaviour
- “Green” assumes a gradual move to pre-pandemic behaviour over the period to March 2022
- “Pink” assumes an immediate step-change to a state close to pre-pandemic behaviour, with a full return to pre-COVID mixing reached by September 2021
In order to see the actual figures more clearly, we have removed the central Imperial projection which indicated much higher levels of hospitalisation than the other models.

This update shows that actual hospitalisations (blue) have started to see a new rise in recent days. They are tracking between the Warwick “green” model projection, which is towards the lower end of the trajectories produced in the initial modelling papers and the LSHTM central projection. Current hospitalisations are actually higher than the Warwick “pink” projection, although that estimate was assumed to peak much earlier and at a much higher level than was seen in the summer.
We will continue to track the figures regularly.
Data
Excess Deaths Study (link)
The ONS has released a study covering excess deaths over the period from the start of the pandemic until 2 July 2021. An emphasis in the report is establishing the extent to which forward displacement of mortality has occurred, which is the notion that many people who died of COVID would have died soon anyway.
The study shows that whilst the periods of low COVID prevalence (and thus mortality) have seen dips in mortality below expected levels, these are minor compared with the excesses seen in the prior peaks.
By early July, when the analysis stops, the overall excess mortality is put at 6% across the 16 months.
Were the analysis to have continued through the summer, we would expect the curve to have turned upwards again given the excess mortality seen, as reported weekly in the CMI’s Mortality Monitor updates (link).
REACT Infection Study (link)
After a pause of two months, REACT has published Round 14 of its infection surveillance study for England. Covering the period 9 to 27 September the results are a little dated, but suggest an R of “around 1” during that period. Within that there is a clear upward trend in children, offset by falls elsewhere.
Overall prevalence for the period is put at 0.83%, notably lower than the equivalent ONS estimates for the same period of around 1.2%.

The other notable insight is evidence that vaccine efficacy starts to wane after around 3 months, and further data that confirms that the AZ vaccine is less effective at preventing infections than Pfizer, with efficacy figures of around 45% and 70% respectively.
ONS Infection Survey (link)
The latest infection prevalence data from the ONS shows a contrasting picture between England and Wales, where they are rising rapidly, and Northern Ireland and Scotland, where the last two weeks have seen significant falls.

Further down the report we see that in England and Wales it’s older schoolchildren who are driving this increase, with some remarkable prevalence figures of 8% and 10% respectively.
“R” Estimate
The latest estimate from UKHSA for England is in the range 0.9 to 1.1, only slightly up from 0.8 to 1.1 two weeks ago.
The regional estimates are shown to the right.
It’s possibly surprising that the estimate is not more equivocally suggesting a rate above 1 given the ONS infection numbers reported above. In particular the ONS view of levels in the South West is firmly that rates are increasing in contrast to the more uncertain picture suggested by the UKHSA estimate.
Other
House of Commons report on lessons learned from the pandemic
This week MPs from the cross-party Health and Social Care and Science and Technology committees released a report reflecting oral evidence sessions held and written submissions received over the course of late 2020 to June 2021. Most of the evidence relates to the first wave of the pandemic.
The stated purpose of the report is to provide an early assessment of the key decisions, structures and underlying factors which contributed to the pandemic’s impact in the UK. The main intention behind the recommendations is to inform future pandemic and other emergency responses.
The report considered six key areas:
- Prior pandemic preparedness
- Deployment of non-pharmceutical interventions
- Testing and contract tracing
- Impact on the Social Care sector
- Disproportionate impacts on some communities
- Vaccine roll-out and use of therapeutics
At 147 pages, the report goes into a lot of detail. The conclusions include elements that went well in addition to the areas where there were significant shortcomings. Recommendations include the need for funding, having appropriate government structures as well as improved interaction with structures and resources outside of government.
And Finally …
With travel restrictions in place, campervans provide a way of travelling with the family and are currently very popular in Hidaka of Saitama prefecture, a suburb to the west of Tokyo. The traditional VW camper features heavily in this collection of happy campers!





