
Weekly Report: Issue 49
By: John Roberts, Matt Fletcher, Dan Ryan & Adele Groyer
COVID-19 Actuaries Response Group – Learn. Share. Educate. Influence.
COVID-19 is still one of the hottest topics for scientific papers and articles. The COVID‑19 Actuaries Response Group provides a regular weekly update with a summary of key papers and articles.
Vaccination
Vaccines (first dose) for 16-17 year olds (link)
Following safety approval for use of the Pfizer vaccine between ages 12 and 17 two months ago by the MHRA, and a previous recommendation by the JCVI to limit vaccination at those ages to those with particular medical needs, the JVCI announced on Wednesday its advice that all 16 and 17 year olds should be offered a first vaccine dose.
For ages below 16 the risk/benefit analysis is said to still be unclear and further data is awaited to make a firm decision. Only the Pfizer vaccine will be used for this extension, with neither the Moderna or AstraZeneca vaccine having approval below age 18.
The explanation for recommending only a first dose at this stage relates to the risk of inflammation of the heart, which is said to occur primarily after the second dose. Again, further data is awaited to allow a recommendation to be made; this is expected within the normal timescales that any second doses would become due.
More evidence that delaying second doses improves antibody response and efficacy (link)
A paper published last week reported on analysis on the impact of delaying the second doses beyond the originally recommended three weeks interval. Whilst the primary reason for the delay was to enable larger numbers of people to receive some protection earlier, a secondary effect has been to improve the eventual antibody response after the second dose.
Due to the decision to extend the time period being taken before AZ vaccinations started, there is a smaller spread of intervals, so the main interest is in respect of the Pfizer vaccine, where trials (and thus the recommended interval) had only been conducted using a three-week interval.
The results show a very marked improvement in antibody response for Pfizer between those ‘second dosed’ at the 3-week point and those for whom the interval was extended to around 11 weeks, thus vindicating the decision to extend the dosing period.
Also of note is that Pfizer responses are generally stronger than for AZ, and that those who had previously been infected gave the strongest responses of all (again with Pfizer exceeding AZ).
Features of SARS-CoV-2 Delta variant vaccine-breakthrough infections (link)
In this pre-print study, the authors performed a retrospective cohort study of patients in Singapore who had received a licensed mRNA vaccine and had been admitted to hospital with Delta SARS-CoV-2 infection. They compared the clinical features, virological and serological details between fully vaccinated and unvaccinated individuals.
Of 218 individuals with Delta infection, 84 had received a mRNA vaccine (71 of these were fully vaccinated), 130 were unvaccinated and 4 received a non-mRNA vaccine. The odds of severe COVID‑19 requiring oxygen supplementation was significantly lower following vaccination (adjusted odds ratio 0.07. CI: 0.015-0.335). PCR cycle threshold (Ct) values were similar between both vaccinated and unvaccinated groups at diagnosis, but viral loads decreased faster in vaccinated individuals.
The authors conclude that mRNA vaccines are highly effective at preventing symptomatic and severe COVID-19 associated with Delta infection. Vaccination is associated with faster decline in viral RNA load and a robust serological response.
Impact of vaccines on hospitalisations in England (link)
Public Health England has updated its estimate of the number of hospitalisations averted by vaccination by considering vaccine effectiveness against hospitalisation, vaccine coverage and observed hospitalisations.
PHE estimates that up to 25 July 2021 around 66,900 hospitalisations have been prevented directly in those aged 65 years and over as a result of the vaccination programme. As there were a total of almost 99,000 hospitalisations of over-65s in that period, the PHE estimate suggests that around 40% of hospitalisations have been averted by the vaccine rollout.
This figure would likely be higher if the indirect effects of reduced transmission could be quantified.
Behavioural nudges to increase COVID-19 vaccination take-up (link)
In this accelerated preview version of a study, the authors report on the results of two sequential large-scale randomised controlled trials (RCTs) that investigate whether nudging people to get vaccinated via reminders can improve COVID-19 vaccine uptake. They further examine the benefits of combining reminders with additional interventions.
UCLA Health, a large academic health system in California, invited patients eligible for a COVID-19 vaccination at the time to get vaccinated. Patients were automatically enrolled in the first RCT if they had not yet registered for a vaccine appointment by the first reminder date (n = 93,354). All patients who had still not registered for an appointment after the second reminder were enrolled in the second RCT (n = 67,092).
Reminders were sent by phone text and all reminders included an easily accessible link to an appointment scheduling website.
Sending the first reminders boosted appointment bookings within 6 days by 6.1% and within 4 weeks by 3.6% compared with a randomly assigned holdout arm that received no reminder. Second reminders increased these outcomes by 1.7% and 1.1% respectively.
The first reminder was more impactful when it was combined with a message that made patients feel the vaccine was already theirs. This was done with statements that the vaccine had “just been made available for you” and encouraged patients to “claim your dose.”. However, the authors found no evidence that combining this message with video information addressing vaccine hesitancy heightened its effect.
These findings highlight the value of making vaccination bookings easy and inducing feelings of ownership.
How long will vaccines continue to protect against COVID-19?
A recent SAGE paper (link) was published on 30 July which considers how long vaccines are likely to protect against COVID-19.
Amongst the findings were:
- Vaccine-induced immunity to infection and potentially severe disease are highly likely to wane over time;
- Re-vaccination against SARS-CoV-2 is likely to be needed for many years, though the optimal frequency needed to protect the vulnerable is unknown;
- Different vaccines may induce different forms of immunity;
- Further and longer longitudinal studies are likely to be needed – in particular, focused studies of individuals where waning of protection is likely to happen sooner.
Clinical and medical news
Immunosuppression and variants of concern (link)
A number of studies have highlighted the risk of multiple viral mutations in immunosuppressed patients who have suffered prolonged infections of SARS-CoV-2. Such patterns of multiple viral mutations are seen in the variants of concern, and implicates infections in immunosuppressed patients in their emergence.
It is worth highlighting quite how much longer these patients are suffering infection (compared with typical COVID-19 patients), with the virus undergoing extensive evolutionary adaptation. One of the patients (Choi) had a sustained infection for 152 days during which time 31 substitutions were observed, whilst another (Kemp) was sequenced frequently over 102 days with increasing rates of substitutions over the period. In both cases, variant viruses that were able to escape the immune response were identified.
The paper highlights the importance of immunocompromised patients with COVID-19 observing self-isolation whilst virus continues to be shed, and alerts to the possibility of reactivation. Household members and close contacts should be vaccinated, although this will be incomplete until there is further investigation and guidance regarding vaccination for children at younger ages. The use of monoclonal antibodies may bolster the immune response and reduce the period of shedding, although the paper notes that there may be reduced effectiveness of monoclonal antibodies such as bamlanivimab and casirivimab against escape variants based on evidence from in-vitro studies.
Type 2 diabetes treatment added to RECOVERY trial (link)
The RECOVERY trial continues to investigate the potential benefits of new and repurposed treatments, with the announcement on 28 July that Empagliflozin is to be evaluated. Empagliflozin is routinely used to treat type 2 diabetes, with benefits for those suffering from chronic kidney disease and heart failure. It is expected to have a range of effects through stabilising metabolic pathways that will reduce inflammation, improve cardiovascular function and improve oxygen transport. The DARE-19 trial (link) investigated a similar treatment, Dapagliflozin, but the size of the trial meant that the benefits in reduction in mortality and organ failure were not found to be significant.
In the proposed trial, 2,500 patients will be randomly allocated to receive Empagliflozin plus usual standard of care. Over the next few months, the trial will investigate whether the treatment shortens length of hospital stay and the risk of needing mechanical ventilation, as well as mortality risk.
Durability of immune memory after SARS-Cov-2 infection (link)
In this study 254 patients in the USA, mostly with mild-to-moderate COVID-19, were evaluated longitudinally starting with recruitment from early April 2020. The cohort will eventually be followed for 2 to 3 years but the authors have reported the results of follow-up for up to 250 days.
This study shows that most COVID-19 patients induce a wide-ranging immune defense against SARS-CoV-2 infection, encompassing antibodies, memory B cells, CD4+ T cells and CD8+ T cells. The immune response to natural infection is likely to provide some degree of protective immunity even against SARS-CoV-2 variants because the CD4+ and CD8+ T cell epitopes will likely be conserved.
This has implications for vaccines which may be more efective if they can induce production of CD8+ T cells targeted on the more stable SARS-CoV-2 nucleocapsid, rather than just to SARS-CoV-2 spike antigens. This may help contain infections as new variants overtake the prevailing strains.
Risk of acute myocardial infarction and ischaemic stroke following COVID-19 (link)
In this study on subjects in Sweden, 86,742 patients with COVID-19 were included, along with 348,481 control individuals who were matched on age, sex and country of residence but who did not have COVID-19 infection.
When day of exposure was excluded from the risk period in the study, incidence rate ratio (IRR) for acute myocardial infarction was 2·9 (CI 1·5–5·6) for the first week, 2·5 (CI 1.3–4·9) for the second week, and 1·6 (CI 0·8–3·0) in weeks 3 and 4 following COVID-19.
For ischaemic stroke the equivalent results were 3.0 (CI 1.7–5.2) in the first week, 2.8 (CI 1.6–4.9) in the second week, and 2.1 (CI 1.3–3·3) in weeks 3 and 4 following COVID-19.
The authors’ interpretation of these findings is that COVID-19 is a risk factor for acute myocardial infarction and ischaemic stroke and suggest that vaccination is needed to reduce these risks.
Efficacy of monoclonal antibody treatment to prevent SARS-CoV-2 infection (link)
REGEN-COV (previously known as REGN-COV2) is a combination of the monoclonal antibodies casirivimab and imdevimab, which has been shown to markedly reduce the risk of hospitalisation or death among high-risk persons with COVID-19.
In this two-part, randomised, double-blind, placebo-controlled trial which was funded by the manufacturers of the treatment, the authors assessed the efficacy and safety of injected REGEN-COV in preventing SARS-CoV-2 infection among previously uninfected household contacts of infected people The trial included 1,505 participants, half of whom were assigned to placebo, and was conducted across 112 sites in the United States, Romania, and Moldova.
Symptomatic SARS-CoV-2 infection developed in 11 of 753 participants in the REGEN-COV group (1.5%) and in 59 of 752 participants in the placebo group (7.8%) (relative risk reduction 81%; P<0.001). REGEN-COV also prevented symptomatic and asymptomatic infections overall (relative risk reduction, 66%).
Progressive increase in virulence of novel SARS-CoV-2 variants in Ontario, Canada (link)
In this pre-print study, the authors report on a retrospective cohort study (using case data February-June 2021) of the virulence of Variants of Concern (VOCs) compared with non-VOC infections. Virulence is measured by risk of hospitalisation, intensive care unit (ICU) admission, and death.
212,332 cases were included. Mixed effects logistic regression models were used to model the outcomes, adjusting for age, sex, time, vaccination status, comorbidities, and pregnancy status.
Compared with non-VOC SARS-CoV-2 strains, the adjusted elevation in risk associated with N501Y-positive variants (Alpha, Beta and Gamma) was 52% (43-62%) for hospitalisation; 89% (67-116%) for ICU admission; and 51% (30-74%) for death.
Increases with Delta variant were more pronounced: 108% (80-138%) for hospitalisation; 234% (164-331%) for ICU admission; and 132% (47-230%) for death.
The authors conclude that progressive increase in transmissibility and virulence of SARS-CoV-2 VOCs will result in a significantly larger, and more deadly, pandemic than would have occurred in the absence of VOC emergence.
Modelling
SPI-M-O: Statement on their concerns for next few months
SAGE’s Scientific Pandemic Influenza Group on Modelling, Operational Subgroup (SPI-M-O) issued a statement (link) on their concerns for the coming months – this was published on 30 July, reflecting their position as at 14 July (i.e. before the move to step 4 of the Government’s roadmap on 19 July).
This provides a helpful summary of the key concerns for the remainder of 2021 and the start of 2022.
The key areas considered are:
- High incidence and prevalence of infection – speed of spread, changes in testing behaviour, implications on workforces and infrastructure;
- Impact of high prevalence on vaccine effectiveness and coverage;
- Reliance on population immunity;
- Autumn / Winter 2021/22 (in particular, schools re-starting and SARS-CoV-2’s interaction with other infectious diseases);
- Novel variants;
- Global surveillance;
- Data availability (especially linked data on vaccination status and hospital admission).
Monitoring actual and modelled hospitalisations
We first monitored hospitalisations in England against projections in Friday Report 48 (link). This updated our bulletin (link) summarising papers from London School of Hygiene and Tropical Medicine (LSHTM), Warwick University and Imperial College London which modelled the move to step 4.
The chart below shows an updated trajectory of actual hospitalisations in England against four of the projections produced by the groups:
- LSHTM central model (assuming waning immunity of 15% over the next 12 months)
- Imperial central model
- Warwick “green” and “pink” models which represent the two extremes of their assumptions on precautionary behaviour
- “Green” assumes a gradual move to pre-pandemic behaviour over the period to March 2022
- “Pink” assumes an immediate step-change to a state close to pre-pandemic behaviour, with a full return to pre-COVID mixing reached by September 2021
This update shows that actual hospitalisations (blue) have reached at least a temporary peak. They are tracking slightly below the LSHTM estimate and broadly in line with the Warwick “green” estimate for early August, which is towards the lower end of the trajectories produced in the initial modelling papers.

We will continue to track the figures regularly.
Data
ONS Infection Study (link)
The latest data from ONS shows that infection levels in three of the four UK countries have started to decline following the reduction in cases we’ve seen since mid-July. The exception is Northern Ireland, where two factors may be behind the continuing increase.
First, as noted in the next item, antibody levels amongst younger adults are noticeably lower in NI. But in addition, July 12th celebrations may have triggered an upsurge in cases, which we have seen in the last two weeks.
ONS Antibody data (link)
The latest fortnightly analysis by ONS on antibody levels in adults now shows that all four countries have levels above 90%, with England slightly ahead on 94%. Northern Ireland is lowest at 91%, and judging by the age profiles, appears to have had more difficulty in persuading younger adults to come forward.
The only age group in England below 90% is now the 16-24 group, which is on 80%. This is unsurprising, as first dose vaccination has only recently finished for those coming forward promptly, and those below 18 have not yet generally had the opportunity to be jabbed (although this will shortly change, as noted earlier in our report).

Long COVID Study Summary (link)
A recent SAGE paper published summarises the results from four different studies into the extent of Long COVID (‘LC’) symptoms, including the familiar ONS, REACT and Zoe studies. With much more complexity around variability of symptoms, duration, and indeed how one assesses whether someone is suffering from it, it’s helpful to have a summary in one place, as results vary considerably.
As shown in the table below, estimates of LC after 12 weeks range from around 2% of those infected to 14%, (with the 0.3% figure being based only on primary care records, which might imply that many cases are relatively mild and have not been raised with the GP).
The high risk factors noted are typically consistent with those for infections and more serious illness, death, with the exception of females (the opposite of what we have seen for mortality, where males have been much harder hit).
REACT infection study (link)
The latest REACT infection study is uncharacteristically out of date, the end point being 12 July. Given the rapid fall we’ve seen since then in cases, it’s thus of less value than usual. However, there are still some useful nuggets of information within it, most notably that of infections by vaccination status.
The study shows that, after adjusting for confounding factors, someone who is doubly vaccinated is less than half as likely to be infected as an unvaccinated person. Moreover, if they are infected, the level of infection they have is considerably lower. Both these factors will of course be instrumental in reducing the transmission risk, and thus reinforces the benefit of vaccination in reducing “R”.
On the infection level point, it should be noted that data published today by PHE is much more uncertain, demonstrating that it is always preferable to look at multiple data sources to get several views.
The other point to note regards the link between infections and admissions/deaths, previously seen to have weakened following the vaccination programme. Recently this weakening appears to have stalled, and indeed there are signs that the impact of Delta may have been to reverse the situation. A contributing factor at younger ages is likely to be that fewer people are vaccinated, either through hesitancy or simply their later place in the vaccination programme.
COVID-19 Health Inequalities Monitoring for England (CHIME) (link)
The CHIME tool brings together data relating to the direct impacts of COVID-19, for factors such as mortality rates, hospital admissions, confirmed cases and, most recently added, vaccinations for people aged 50 and over.
Inequality breakdowns are provided, including by age, sex, ethnic group, level of deprivation and region. For vaccinations, denominators are the National Immunisation Management Service (NIMS) data set which has been linked to the Office for National Statistics (ONS) Public Health Data Asset (PHDA) based on NHS number. The ONS PHDA is a unique linked dataset combining the 2011 Census, the General Practice Extraction Service (GPES) data for pandemic planning and research and the Hospital Episode Statistics (HES).
As at June 2021:
- 87% of people aged 50 to 59 were fully vaccinated with 2 doses, up to almost 96% for ages 70+;
- 85% of London residents were fully vaccinated compared with 91-94% in other regions;
- 87% in the most deprived quintile were fully vaccinated, v. 95% in the least deprived quintile;
- Take-up rates (TURs) are lower among those who rent housing (83% to 85%) compared with take-up rates among those who own their homes (94%);
- TURs are lowest among the long-term unemployed (79%) while there is a narrow range (91% to 94%) for all employed people classified by NS-SEC;
- TURs are only slightly lower among people with the most limiting disability status compared with those with no or limited day-to-day limitations (89% vs 92% respectively);
- There are wide disparities in take-up by ethnic group with the lowest TURs among people of Black Caribbean ethnicity (65%), and the highest among people of White British ethnicity (94%).

- Full vaccination TURs are 82% among people born outside the UK, compared with 93% for those born in the UK;
- TURs are lowest at 73% for those with no English language proficiency, compared with the highest TURs of 93% among those whose main language is English;
- By religion, TURs are lowest among Muslims (76%), followed by “other” religions (81%) and Buddhists (83%). All other religions cluster between 89% and 93%.
The widest disparities are correlated with ethnicity and country of birth which could lead to unequal health outcomes by these factors unless more can be done to encourage take-up.

There was progress in take-up between May and June 2021 but the data up to 1 August 2021 reported in the Weekly National Influenza and COVID-19 surveillance report (link) does not suggest that any progress has been made in terms of ethnicity differentials among over 50s since June.
“R” Estimate
 Over the last two weeks the estimate of R published by the UK Health Security Agency has fallen sharply. From 1.2 to 1.4 a fortnight ago, a modest fall last week to 1.1 to 1.4 has now been followed by a much bigger fall to 0.8 to 1.1, implying a central estimate below 1 for the first time in nearly three months.
Over the last two weeks the estimate of R published by the UK Health Security Agency has fallen sharply. From 1.2 to 1.4 a fortnight ago, a modest fall last week to 1.1 to 1.4 has now been followed by a much bigger fall to 0.8 to 1.1, implying a central estimate below 1 for the first time in nearly three months.
The regional picture is shown to the right.
Other
Improvement in contact tracing through use of machine learning (link)
There continues to be significant debate over the effectiveness of different contact tracing approaches following the decision to reduce the number of potential “pings” by reducing the period of tracking potential contacts with Bluetooth technology in the UK from 5 days to 2 days.
A university in MidWest USA has investigated two machine learning models to predict which students are at elevated risk of contracting COVID-19. 2.9% of the cohorts selected by the adaptive machine learning models were positive within 14 days of selection as compared with 1.3% of a random cohort. Further, close contacts predicted by the models received a COVID-19 test within 0.9 days of the source testing positive as compared to close contacts who were manually contract traced being tested within 1.9 days.
These results show the potential value of adaptive machine learning models to distribute testing resources efficiently and prevent onward transmission.
And finally …
Professor Sarah Gilbert has, deservedly, not been short of accolades this year, including being made a Dame in the recent Honours list, and a standing ovation on Centre Court at Wimbledon.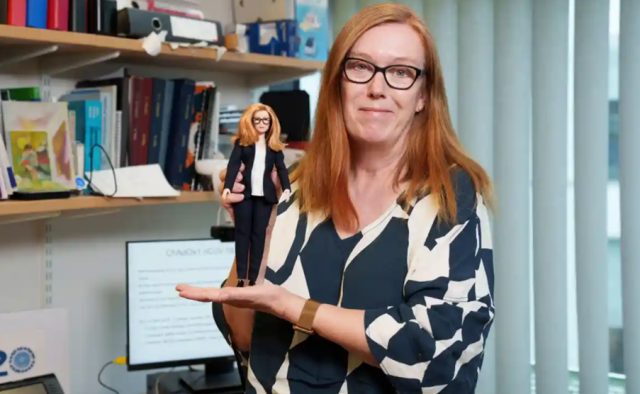
Her latest accolade is from the toy firm Mattel, which has made a Barbie Doll in her image, along with five other women working in Stem around the world.
Dame Gilbert commented that she hoped it would inspire young girls to consider a career in Stem, and make them aware of careers that they may not be aware of.
We are now wondering who will be the male equivalent, should Mattel’s ‘Ken’ line need a vaccinology update …
6 August 2021



